The uptick in the tick population across the United States is of greater concern than ever.
According to the Centers for Disease Control, deer ticks, which can transmit Lyme disease, infected as many as half a million Americans last year with a type of bacterium that is hard to diagnose and even harder to treat.
Now, Tulane University researchers have found that a tick bite can lead to such persistent infections that traditional antibiotics may not ever completely eradicate the disease.
And when the bacteria — Borrelia burgdorferi spirochetes — from the Lyme-infected deer tick enter the human bloodstream, the disease can spread to other parts of the body, and even may cause a severe form of dementia.
Ticks have migrated from their usual stomping grounds of the Northeast and Midwest and are now invading the South and northern California, among other states, in smaller but very real numbers. The ticks feed on white-footed mice and birds, which have become efficient carriers. And with climate change, longer summers mean more time for the tick feeding season.
Initial Lyme disease symptoms can include headaches, fever, fatigue and a rash. Untreated Lyme can affect the joints, the heart and the nervous system. But many people who’ve come in contact with ticks are unaware they’ve been bitten or infected.
“Once your bloodstream is contaminated, the spirochetes begin to move quickly into your joints and other organs,” said Dr. Monica Embers, associate professor of microbiology and immunology, and lead researcher on Lyme at the Tulane National Primate Research Center in Covington.
“Once the spirochetes have invaded organs, they can cause everything from arthritis and Bell’s palsy to very complex neurological problems,” she said.
The number of confirmed cases of Lyme disease in Louisiana is very small — just eight in 2019. But for Louisiana residents who have been diagnosed with Lyme, finding treatment can be frustrating. Doctors here have less experience with the disease than those in states where it's more common, like Pennsylvania or New York.
Lyme is underreported
Buffie LaRocca, of Mandeville, has been frustrated finding care in Louisiana.
“We’re often called the Lyme loonies because much of the medical community here doesn’t believe we have contracted Lyme in this state," LaRocca said. "And with a small patient base, (doctors) would rather not treat us, suggesting we go to places like Johns Hopkins which have more experience” and doctors versed in treating Lyme disease.
Dr. David Mushatt, a Tulane infectious disease specialist, said tests to confirm Lyme are complicated, often requiring out-of-state labs. Doctors are busy seeing patients and have little time to report cases to public health entities, which is supposed to be the job of labs. Such underreporting is, apparently, rampant. While 30,000 cases are reported by state health authorities to the CDC annually, the federal public health agency estimates that 476,000 people are infected with Lyme every year.
Sheila St. Romain was diagnosed with Lyme in 2008 in Alexandria, where she believes she was bitten. Her blood was sent to a respected lab in California, and later she tested positive at Ochsner, where she’s being treated.
“It’s been a nightmare,” said St. Romain. The long-term effects of Lyme can be devastating. "I’ve been on an enormous amount of antibiotics, but at this point I'm bedridden after having had both a heart attack and a stroke, and now my muscles are atrophying. My last test for Lyme was negative, but the horrible symptoms linger.”
Sometimes, definitive answers come only after death. When a 69-year-old woman with persistent Lyme symptoms for 15 years experienced continual neurological decline, her decision to leave her brain to Columbia University illuminated just how far-reaching the consequences of Lyme disease can be.
Eventually, the woman succumbed to Lewy body dementia, which causes impaired thinking, along with movement and psychotic mood disorders. Upon autopsy, Embers and her lab found Lyme spirochetes in the woman’s spinal cord, despite years of antibiotic therapy. These findings were published in Frontiers in Neurology, a joint study between Tulane and Columbia Universities.

Rhesus monkeys at the Tulane National Primate Research Center near Covington.
Testing new drugs
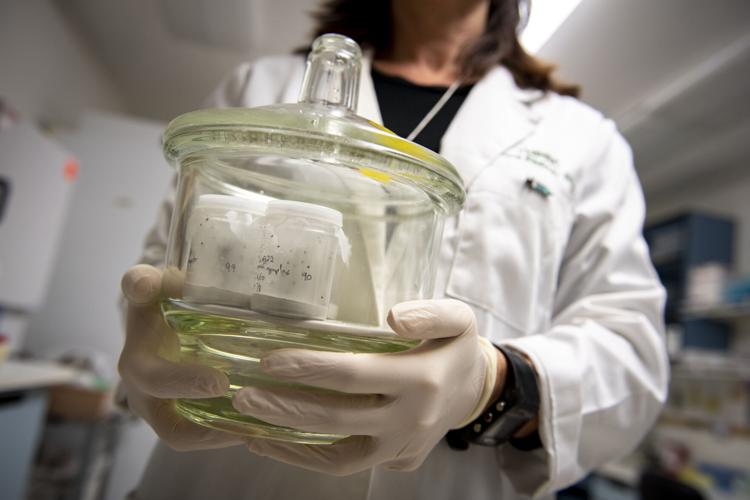
The primate center is using rhesus macaques, a species of Old World monkey, to help determine which treatments work to eradicate Lyme infections before symptoms become chronic, Embers said.
“Our lab is now testing a triple drug treatment, consisting of three different antibiotics given simultaneously. It’s been shown to be effective in mice, but the key will be to determine its efficacy in the primates,” she said.
According to Embers, the biggest challenge is to figure out when the infection has cleared the body, because it hides out in the joints and isn’t always detectable in urine or blood samples.
So, to outsmart the elusive Lyme infection, rhesus macaques are infected and then treated to cure the infection. Next, uninfected ticks are allowed to feed on the monkeys. If the monkey is still infected despite the regimen of antibiotics, the tick will take in bacteria. After feeding, the tick is examined, to see if it is carrying the bacteria.
Immune systems gone awry?
Dr. Julio Figueroa, infectious disease specialist at LSU, hopes that new research might prove that rapid, multiphase treatment after the initial bite will head off problems later.
“These long-term post-inflammatory effects are much like we’re now seeing in COVID patients who are no longer positive but suffer terrible aftereffects," Figueroa said. The doctor said he recently found a tick on his skin and gave himself a precautionary dose of antibiotics. But, he said, "I am reluctant certainly to give any long-term dose of antibiotics to my patients, as there are a multitude of side effects in aggressive treatment which can destroy the biome and kill off one’s good bacteria.”
Without a test, diagnosis is tricky. The classic bull's-eye rash indicating Lyme doesn’t appear in 20% to 30% of people who’ve become infected, delaying their treatment until more serious symptoms appear, which could be late in the game.
Making matters worse, the ticks that transmit Lyme are very small, Embers said. “If you take a pen and make a dot on your paper, that’s how small they are. And, when they’re questing (for food), they will crawl out to the very tip of a leaf to get to you when you pass by.”
Women who have chronic Lyme disease can pass that infection on to their children in the womb. And it's now known that ticks also carry Bartonella (cat scratch disease), which can cause ongoing inflammation and lead to serious health problems.
“A lot more research needs to be done to determine if long after the Lyme infection is gone, the inflammation persists,” Mushatt said. “If our immune systems have gone awry after these infections, then antibiotics will not be the answer for chronic, persistent symptoms, and we need to figure out what will work.”
Email Leslie Cardé at lesliecardejournalist@gmail.com.