The omicron wave has peaked in Louisiana.
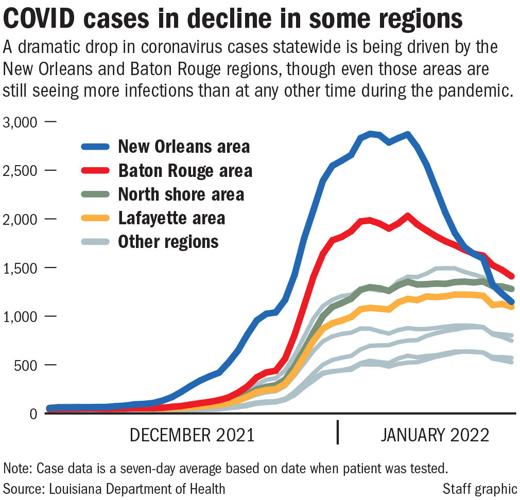
In recent days, the number of new cases of COVID-19 in the state have steadily fallen from the all-time high of 81,305 weekly reached the week ending Jan. 8. However, health experts said the declines are driven by sharp drops in Baton Rouge and New Orleans, the state's most populous regions, and warned that cases are still rising elsewhere.
“When you look at the state as a whole, we have peaked,” said Dr. Joe Kanter, the state's top health officer, at a press briefing Thursday. “But there still are a few regions of the state that are going up and we expect will be peaking very soon.”

Kanter said there aren't yet signs of a steady decline in Lafayette, Lake Charles, Alexandria and the north shore. He also warned that passing the peak in daily cases is still a far cry from points earlier in the coronavirus pandemic when cases were very low. There are still hundreds of people in the state's hospitals seriously ill with COVID-19, and the number of people dying each day is still rising.
“When you’re on the other side of the mountain, you can still be awfully high up off the ground, which is where we are now,” said Kanter.
Even as dropping case counts in New Orleans and Baton Rouge have helped to pull down statewide numbers, there is far more COVID circulating in the state than at any other point in the pandemic: the level of infections remains roughly 60% higher than anything seen before.
Public schools in New Orleans and Jefferson Parish reported a sharp decline in positive COVID cases this week, the latest indication that they…
The story is similar when looking at counts of patients hospitalized with COVID, which serves as a measure of both the severity of the infections and the strain the pandemic is taking on health care resources.
The omicron wave appears to have peaked statewide last week, when about 2,300 people who were infected were in hospital beds. By Thursday, the number of hospitalized patients fell to 2,187.
That’s a dramatically lower rate than was seen during delta, when hospitalizations reached 3,022. More people were protected by vaccines during this wave, or had prior infections that may also have afforded some protection. Also, studies suggest omicron was milder than earlier variants.
As with cases, the fall in hospitalizations has been driven largely by falling case counts in New Orleans, Baton Rouge and Shreveport, though some of those declines are because deaths – which lag infections by weeks – are only now starting to increase.

People receive free COVID-19 test and KN95 masks at an event on the 600 block of Fulton Street sponsored by the New Orleans Health Department, Louisiana Department of Health and Mako Medical in New Orleans, La. Thursday, Dec. 30, 2021. (Photo by Max Becherer, NOLA.com, The Times-Picayune | The New Orleans Advocate)
There have been 1.1 million confirmed and probable coronavirus infections in Louisiana since the beginning of the pandemic two years ago, which would translate to about one in every four residents having contracted it at some point. While some of those confirmed cases are likely re-infections, many other people may have contracted the virus without knowing it, or may have never gotten a test.
The wave of cases driven by the highly-infectious omicron variant, which arrived in Louisiana in early December, was responsible for more infections than any other wave.
In the 46 days since cases started rising, there have been 227,168 confirmed cases. The delta wave, which hit this summer, lasted 104 days, there were 191,725 confirmed cases.
An additional 4,759 confirmed cases were reported Thursday by the Louisiana Department of Health.
Omicron hit just as many people were gathering for the holidays. With few restrictions in place, it quickly swept through many families and workplaces. Hospital systems and health care providers were among the hardest hit.
With isolation putting many nurses, doctors and other workers out of commission, hospitals were again stressed by the surge in patients, even if numbers didn't reach levels seen earlier in the pandemic.
“There are a lot of folks who are very burned out,” said Dr. Julio Figueroa, chief of infectious diseases at LSU Health Sciences Center New Orleans. “And that concerns me a lot.”
New Orleans health director Dr. Jennifer Avegno decided not to ride as queen of Krewe du Vieux next month after unspecified threats that cause…
At Ochsner Health, the state’s largest hospital group, a total of 698 employees were out due to COVID at the beginning of this week. That’s down from a high of around 1,400 out sick in late December, according to Ochsner CEO Warner Thomas.
Ochsner is also reporting an encouraging drop in COVID patients in its facilities. As of Monday, about 644 patients systemwide were hospitalized with COVID, down from a peak of 726 two weeks ago.
The downward slide in cases and hospitalizations comes just ahead of the busiest weeks of the Carnival season, when people across the state will gather for parties, parades and other revelry. Tens of thousands of tourists are likely to descend on New Orleans for parades that will roll for the first time since 2020, and balls and other gatherings are in full swing.
The increased travel into New Orleans and the size of crowds may mean that COVID cases don't see the same steep decline as in other cities and countries hit earlier by omicron.
“Visitors from all over world, certainly all over the country come,” Figueroa said of Mardi Gras in New Orleans. “Whatever is out and about in the country is going to come here and cause issues.”
In New Orleans, the weeks before Mardi Gras lead to an increase in hospitalizations during non-COVID times, said Susan Hassig, an epidemiologist at Tulane University.
There are more accidents of all sorts, fights and hospitalizations related to alcohol intoxication. Regardless of whether omicron is losing steam, a COVID wave followed by an influx of people due to more activity could strain an already stressed system.
Gov. John Bel Edwards flew to the nation's Capitol on Wednesday, but Louisiana politicos shouldn't expect to see him partying it up at Washing…
“We’ve got to hope and pray our hospitalization numbers are way, way down,” said Hassig. “We need to give the health care workers at least a week or two to recoup a little bit of energy, their resiliency and their resources to be able to handle what’s going to start showing up in the ER in about a month.”
Hassig also warned that the end of omicron does not mean the end of COVID. In the short run, Hassig expects another wave in summer, as has been the pattern when people in this region go inside during the hotter months.
“My sense is that something is going to pop in the southern belt, as long as we remain substantially unvaccinated, every six months,” Hassig said, referring to the low global vaccination rate that allows for the likelihood of new variants as well as Louisiana’s relatively unvaccinated population.
About 52% of the state’s population is fully vaccinated, with 15 parishes reporting that less than 40% of residents have received both doses, according to data from the Centers for Disease Control and Prevention.
More treatments are expected to arrive in coming months that health officials hope will relieve the pressure on hospitals. Louisiana received just 672 doses of the monoclonal antibody that works against omicron this week, which were distributed across 71 hospitals.
That means doctors have been limited in who they can distribute it to, reserving it for only the most at-risk patients who are early in the disease.
By March or April, the supply of sotrovimab, the effective monoclonal, and antiviral pills like Paxlovid, which is a five-day course of pills, should be ramped up, said Figueroa. This week, the state received 1,140 doses of Paxlovid, which was distributed to 57 pharmacies.
“What is ultimately going to change how we interact with this virus long-term is the continued development of antivirals and post-infection therapies that reduce the likelihood of hospitalization,” said Hassig.
When Katie Remes’ New Orleans-area hospital needed nurses to staff a new COVID ward in March 2020, she volunteered. She wanted to be there for…
However, the medications will require both an ample supply of tests to identify infections early and a prescription process, because the antivirals are not without their own problems – they cannot be taken with certain common heart medications or by pregnant people.
Public health experts urged mask-wearing during on ongoing surge.
“I don’t think masks are forever – I don’t even think they’re for this whole year,” said Kanter. “But while we’re in a surge, people need to mask up around other people, particularly indoors.”